Tardive dyskinesia (TD) is a serious and often misunderstood movement disorder that affects thousands of people who take antipsychotic medications. Although antipsychotics are essential for treating conditions like schizophrenia, bipolar disorder, and severe depression, they can, over time, cause unintended and sometimes permanent side effects—including TD.
In this article, we explore what TD is, how it develops, why antipsychotics trigger it, and what patients should discuss with their healthcare providers to reduce their risk.
What Is Tardive Dyskinesia?
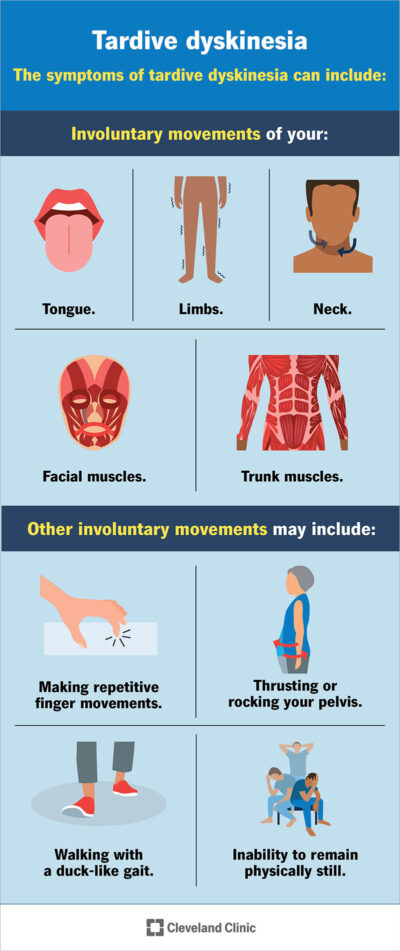
Tardive dyskinesia is a neurological movement disorder marked by uncontrollable, repetitive movements, often involving the face, lips, tongue, hands, or torso. These movements are not voluntary and can range from mild to debilitating.
Common symptoms include:
- Lip smacking or chewing motions
- Tongue thrusting
- Facial grimacing
- Rapid blinking
- Jerky arm or leg movements
- Rocking or swaying of the body
TD develops gradually and may not appear until months or years after starting antipsychotic treatment.
Why Antipsychotics Can Lead to TD
Antipsychotics—especially those that block dopamine receptors—can disrupt normal dopamine activity in the brain. Dopamine is crucial for controlling movement, and when the brain adjusts to long-term dopamine blocking, it may overreact by causing involuntary movements.
Higher-Risk Medications
Certain drugs carry a greater risk:
- First-generation antipsychotics (typical antipsychotics)
Examples: haloperidol, fluphenazine, chlorpromazine
These have the highest association with TD. - Second-generation antipsychotics (atypical antipsychotics)
Examples: risperidone, olanzapine, quetiapine
Lower risk than older drugs, but still significant. - Other dopamine-blocking medications
Example: metoclopramide (used for nausea and GERD)
Long-term use also increases TD risk.
Who Is Most at Risk?
While anyone on antipsychotics can develop TD, certain groups are more vulnerable:
- Older adults
- Women
- People with diabetes
- Individuals taking higher doses or long-term prescriptions
- Those with mood disorders such as depression or bipolar disorder
Risk also increases with duration of exposure, meaning the longer someone uses dopamine-blocking medications, the more the risk rises.
Hidden Risks Patients Should Not Ignore
1. TD Can Be Permanent
Even if the medication is stopped, TD symptoms may remain or worsen. Early detection is critical.
2. Symptoms Can Be Mistaken for Mental Health Issues
Some movements—like restlessness or agitation—are easily misinterpreted as worsening psychiatric symptoms, delaying proper diagnosis.
3. TD Can Affect Mental Health
The social impact of visible involuntary movements can lead to:
- Anxiety
- Embarrassment
- Isolation
- Worsening depression
4. Not All Clinicians Screen Regularly
Despite guidelines, TD screening may not happen routinely unless the patient or family brings up concerns.
Can TD Be Treated?
Yes. Several strategies can help:
1. Medication Adjustments
Doctors may reduce dosage, switch medications, or explore alternatives when possible.
2. FDA-Approved TD Treatments
Two VMAT2 inhibitors are currently approved to reduce TD symptoms:
- Valbenazine (Ingrezza)
- Deutetrabenazine (Austedo)
These medications do not cure TD but can significantly reduce involuntary movements.
3. Supportive Therapies
Physical therapy, stress reduction, and symptom-management techniques can help improve quality of life.
What Patients Should Discuss With Their Doctor
- How long have I been on dopamine-blocking medications?
- Should I be regularly screened for TD?
- Are there safer medication alternatives?
- What early symptoms should I look out for?
- If I already have symptoms, what are my treatment options?
Proactive communication is one of the strongest tools for preventing long-term complications.